Situation:
We are third year nursing students in the Nursing Education Program of Saskatchewan on 6300 neurosciences at Royal University Hospital. The purpose of this blog is to present a case study of a client on the ward during our clinical rotation whom we considered to be a complex patient.
We are presenting this case study to further facilitate our learning of caring for a complex patient on a neurology based unit. We also hope that our experience will provide an opportunity for the visitors to this site to gain a similar knowledge base and understanding by accessing our research, plan of care and various linked resources.
Background:
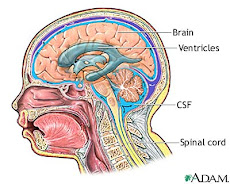
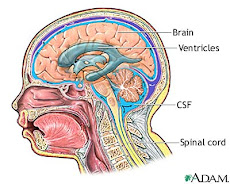
Wilbur Longbottom is an 82 year old male who presented at Saskatoon City Hospital ER on January 30th 2009 with confusion, aphasia and right sided weakness. He was transferred to St. Paul’s Hospital for a head CT which illustrated an intraventricular hemorrhage (IVH) beginning in the left lateral ventricle and expanding to include the third right ventricle and temporal lobe. He also had mild hydrocephalus. He was next transferred to Royal University Hospital (RUH) where an external ventricular drain (EVD) placed to maintain intracranial pressure within normal limits. His blood work demonstrated an increased INR of 4.1 and elevated white blood cells (WBC).
He has a history of atrial fibrillation, gastric ulcers, hypothyroidism, and hypertension. He was on warfarin at the time of admission for treatment of atrial fibrillation.
He remained in the RUH intensive care unit for 5 days. On February 4th, he was extubated but was unable to maintain a patent airway and a #6 cuffed Shiley tracheotomy was placed. On February 5th he was admitted to the observation unit on 6300 with a fluctuating Glasgow Coma Scale (GCS) of between 9 and 11. His GCS has remained fluctuating between 9 & 11 throughout the five days he had been in observation. He had a 3 lumen Foley draining frank hematuria as a result of traumatic insertion and wears benefits for bowel incontinence. He was independent of all ADL’s before this hospitalization. His increased WBC count was also of concern and he was under investigation for query meningitis.
Assessments:
Caring for complex patients is multifaceted and nurses must be competent in general head to toe assessments with the ability to focus each assessment according to the specific needs of the patient. For this patient our focus would be on the neurological system paying specific attention to the Glasgow Coma Scale, LOC, behavioural or physical changes that may indicate increased ICP, and the muscular strength of the patient. Monitoring for signs of infection is also essential as he has an EVD which provides a direct entry into the brain and already has an elevated WBC count. Other key skills for nursing this client include reading ECGs, competent medication management, interpreting blood work and monitoring for signs of clots as he has atrial fibrillation but is no longer on warfarin. We would also monitor for bleeding as he has already experienced a cerebral bleed and has gross hematuria.
Recommendations:
We recommend that other students access the links on this page to gain a better understanding of the diagnostics and procedures involved with Wilbur Longbottom. Many of these procedures are relevant to numerous patients with neurological injuries and disorders and therefore the knowledge from this case can be transferred to other situations, adding to our knowledge base as health care providers.
skip to main |
skip to sidebar
Links
- What are anticoagulants?
- Wafarin information
- Anticoagulants and risk for brain hemorrhage
- INR Quiz
- Article: Kidney Function Influences Warfarin Responsiveness
- Article on insulin and neuro surgery
- Care of EVD
- Complications of tracheotomy
- Hydrocephalus
- E-Book on common ICU errors (monitoring ICP)
- Patient teaching for A-Fib
- Atrial Fibirilation Video
- CT Scan Video
Anotomy of head