In the article, “Case and Care Complexity In the Medically Ill”, defines complexity as multi-morbidity, more specifically as a “complex adaptive system that consists of individual agents with the freedom to act in ways that are not always totally predictable, and those actions are interconnected so that one agents actions changes the context for other agents” (Jonge, Huyse, & Stiefel, 2006, p. 679). Complexity arises when several systems or disease processes interact, sometimes resulting in overlapping symptomology, referred to as case complexity. This article also includes psychiatric co-morbidities, such as frailty and depression, which are often overlooked in the complexity system (Jonge et al., 2006). This model of complexity derives its focus from medical conditions with the interaction of multiple systems along with considerations of psychosocial condition of the client.
Complexity science as defined by Wilson , Halt & Greenhalgh (2001) suggests that illness results from complex and unique interactions in both the physical and psychosocial systems; any small differentiation in any one system will cause an imbalance throughout the remaining systems. Interaction between the systems is the cause of disease complexity, not just a single components malfunction. It also suggests that we as care providers have to take a more holistic approach in our treatment towards our clients. The holistic approach is looking at the relationships between interacting body systems, the behaviour, the environment and the beliefs of the patient which are dynamic and fluid.
Comparing the perception of complexity between these two articles, similarities are apparent at first, yet differences arise with further analysis. Comparing similarities, each focuses on systems interactions as the cause of complexity within the patient. Wilson et al (2001) states, “Human beings can be viewed as composed of and operating within multiple interacting and self adjusting systems (including biochemical, cellular, physiological, psychological, and social systems)” (p. 685). Jonge et al (2006) have a similar perception as they also focus on the interactions of systems which then in turn results in patient complexity.
Differences with these two definitions of complexity stem from the specific considerations of systems interactions. Jonge et al (2006) incorporates main body systems as the interacting determinants for complexity, more specifically psychological and somatic medical issues. One specific example used is the relationship between metabolic syndrome, depression, and cardiovascular disease which focused on the physical ramifications of these interacting diagnoses. Wilson et al (2001), however has a broader definition and scope for looking at complexity. Although the risk factors and symptoms play a role, a wider perspective including all aspects of the patients past experiences and adaptive responses to their new environment are incorporated (p. 685). Wilson et al (2001) perception is also more consistent with the holistic goals of providing nursing care. As future nurses, identifying the importance to consider the patient in a holistic view will aid in providing improved quality of nursing care as compared to the specific focus on only patient medical diagnosis.
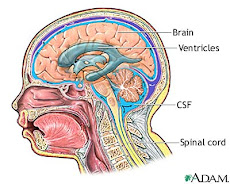
Wilbur Longbottom is an eighty two year old male with a history of hypothyroidism, atrial fibrillation, hypertension, gastric ulcer and “kidney problems”. He has had a cholecystectomy and “fluid in lungs“ in early January, as well as hearing problems. Patient was diagnosed by CT as having an intraventricular hemorrhage, possible cause being an increased INR of 4.1. An EVD was placed to control his intracrainial pressure, and he was then placed in ICU. A tracheostomy was also placed due to his inability to maintain his airway; hematuria is also present due to a traumatic catheter insertion. The patient was then transferred to neurology 6300 after six days in ICU, and has been in observation since the transfer due to a fluctuating GCS. There is also suspicion of query meningitis not yet diagnosed.
This patient matches the presented standard of complexity with his current medical state which include all body systems, interactions among these and overlapping symptomology. In the central nervous system he has intraventrical hemorrhage and problems with fluctuating GCS. In the cardiovascular system his history of atrial fibrillation has led him to be placed on Warfarin; which has caused his increased INR levels, thus IVH, he also has a history of hypertension. He was unable to maintain a patent airway in hospital and because of this his respiratiory system is also affected, he has a tracheostomy, copious amounts of creamy yellow secretions, fluid to bases of lungs, and has been placed on aspiration precautions. This patient has history of gastric ulcers which are being treated with prescription Ranitidne; which is known to interfere with warfarin clearance. Mr Longbottom has also pulled out his NG tube and is awaiting a modified barium swallow test, but until that test he is NPO. In genitourinary he has a three way catheter inserted and has had hematuria related to a traumatic insertion, and is currently using benefits. Mr Longbottom is currently on numerous diuretics for his HTN, this coupled with his history of “kidney problems” puts him at greater risk of kidney failure. His integumentary has been impaired by the surgery, and he has a large incision to his head with an EVD, this device has greatly reduced Mr. Longbottom's mobility which may possibly lead to a breakdown of his skin. The patient has a history of hypothyroidism and is on levothyroxine for this, he is also currently on Humulin R as per standard aftercare of neurosurgery patients. This is because the body has an altered stress response and may not be producing enough insulin naturally.
Sometimes overlooked but equally important are psychological issues the patient is facing (Jonge et al, 2001). This patient is experiencing impaired speech and thus unable to verbalize his needs. He is experiencing frustration due to this as he loved to talk previous to hospitilazation. According to Mr. Longbottom's wife, prior to this admission he was independent and this loss of independence coupled with not being able to do normal ADL's may lead to further frustration for both the patient and his family.
References
Jonge, P., Huyse, F.J., Stiefel, F.C. (2006). Case and care complexity in the medically ill.
The Medical Clinics of North America. 90(1), 679-692.
Wilson, T., Holt, T., Greenhalgh, T. (2001). Complexity science: Complexity and
clinical care.323; 685-688. Retrieved February 23, 2009 from bmj.com.
skip to main |
skip to sidebar
Links
- What are anticoagulants?
- Wafarin information
- Anticoagulants and risk for brain hemorrhage
- INR Quiz
- Article: Kidney Function Influences Warfarin Responsiveness
- Article on insulin and neuro surgery
- Care of EVD
- Complications of tracheotomy
- Hydrocephalus
- E-Book on common ICU errors (monitoring ICP)
- Patient teaching for A-Fib
- Atrial Fibirilation Video
- CT Scan Video
Anotomy of head